What is Follicle Stimulating Hormone (FSH)?
Follicle stimulating hormone, abbreviated FSH (follitropin), is a hormone produced in the pituitary gland – the gland in the brain that controls the body's hormonal balance. FSH plays a central role in the reproductive system of both women and men and affects the function of the ovaries and testicles.
An FSH test is used to measure the concentration of follitropin in the blood and is often included in investigations of fertility, hormonal balance and pubertal development. The test provides important information about how well the gonads are functioning and can help detect hormonal disorders that affect reproductive ability.
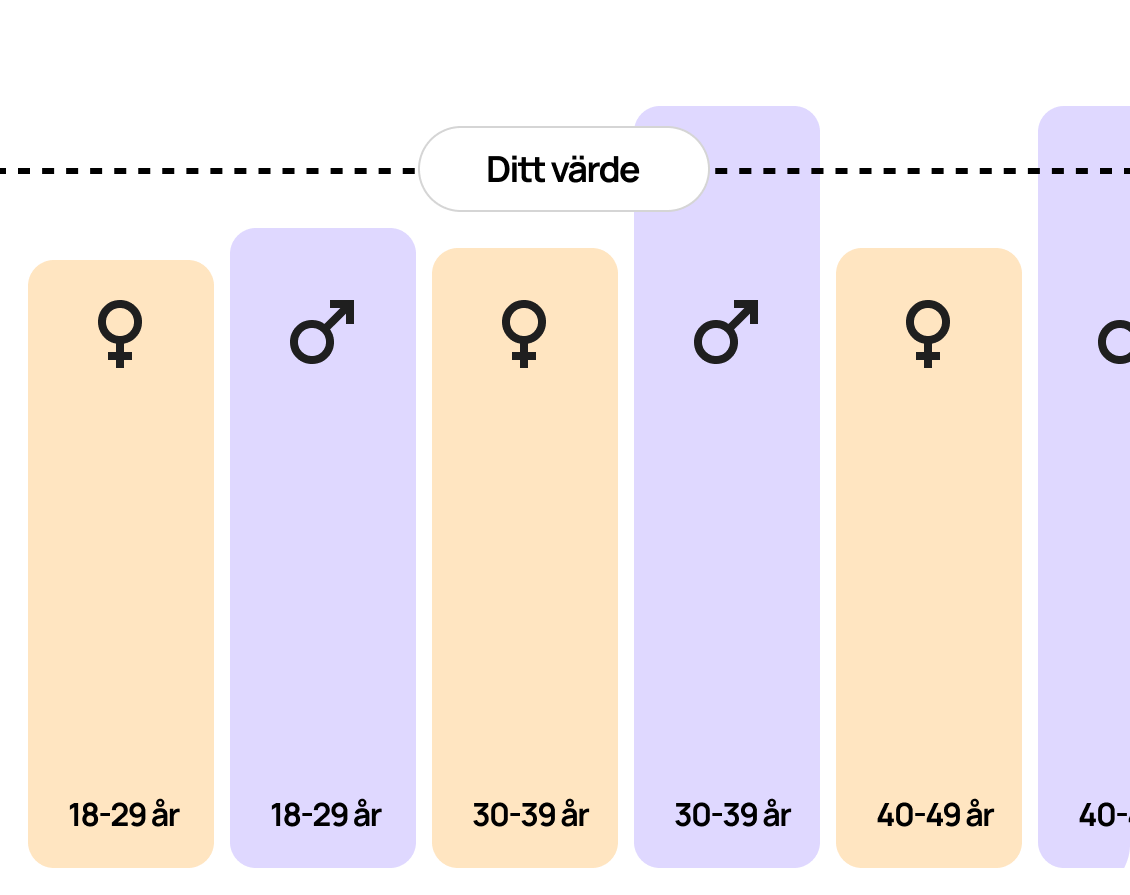
How are FSH results interpreted?
FSH levels are always interpreted in relation to other hormones and the clinical situation. In women, FSH is often combined with luteinizing hormone (LH) and estradiol to assess ovarian function, while in men it is analyzed together with testosterone and sometimes inhibin B to evaluate testicular function.
An FSH test is therefore an important part of fertility investigations and hormonal health checks, and can provide guidance on hormonal imbalances, age-related changes or underlying diseases that affect the reproductive system, but at the same time the analysis is also relevant for men and testosterone concentration.
FSH and testosterone in men
FSH and testosterone are closely related to each other through the hypothalamic–pituitary–gonadal axis. The pituitary gland releases FSH and LH, which signal the testicles to produce sperm and testosterone. FSH stimulates the Sertoli cells in the testicles, which are necessary for sperm production. At the same time, LH stimulates the Leydig cells to produce testosterone. If testosterone levels fall, the pituitary gland tries to compensate by increasing the production of FSH and LH.
In primary testicular failure (impaired function of the testicles), high FSH values are therefore often seen in combination with low testosterone. If both FSH and testosterone are low, it may instead indicate a disorder in the pituitary gland or hypothalamus – a condition called secondary hypogonadism.
- Assessment of ovarian reserve: In women, FSH is used to evaluate ovarian function and egg reserve. Elevated levels may indicate reduced ovarian reserve, which is common during menopause (perimenopause and menopause) or in conditions such as primary ovarian insufficiency.
- Diagnosis of menstrual disorders: Abnormal FSH levels can reveal causes of irregular or absent menstruation (amenorrhea), such as polycystic ovary syndrome (PCOS) or hormonal disorders in the pituitary gland.
- Investigation of menopause: High FSH levels are typical in menopause, as the ovaries no longer respond to signals from the pituitary gland, which leads to increased production of FSH as a compensatory mechanism.
- Infertility: In cases of difficulty in conceiving, FSH together with LH, estradiol and AMH can provide a clearer picture of fertility and facilitate planning of possible treatment options.
- Assessment of testicular function in men: Elevated FSH levels may indicate reduced sperm production, while low levels may indicate that the pituitary gland is not stimulating the testicles sufficiently. The test is therefore often used in the investigation of male infertility.
What affects FSH levels?
- Age: FSH levels naturally increase with age, especially in women after the age of 35.
- Hormonal contraceptives: Can affect FSH and should be avoided before testing if the purpose is to assess natural hormone function.
- Stress and illness: Temporary changes in hormone balance can temporarily affect FSH values.
When should FSH be tested?
For women, testing is recommended early in the menstrual cycle, usually on days 2–5, to assess ovarian reserve and identify any menstrual irregularities, menopausal symptoms, or hormonal imbalances.
In men, FSH testing is used to investigate causes of low sperm production, reduced fertility, or suspected pituitary dysfunction.
Please note: FSH values should always be interpreted in conjunction with other hormone and medical information. A single measurement is rarely sufficient to draw firm conclusions about hormone status or fertility.