What is SLE – systemic lupus erythematosus?
SLE, or systemic lupus erythematosus as the abbreviation stands for, is a chronic autoimmune disease in which the body's immune system begins to attack its own body. Normally, the immune system should protect us against infections. When this happens, it can lead to inflammation in, among other things, the skin, joints, kidneys, lungs and blood vessels. The disease varies greatly from person to person, both in symptoms and how severe it is.
Common symptoms of SLE
SLE is a so-called "systemic disease", which means that it affects several parts of the body. Here are common symptoms of SLE:
- A severe fatigue that is not relieved by rest
- Fever that comes especially during a flare-up or infection
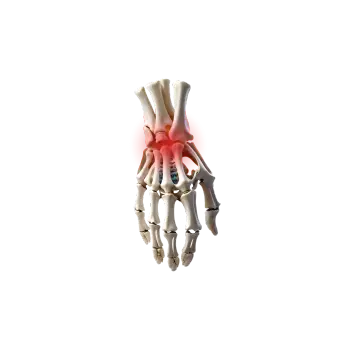
- Stiffness and joint pain that often occur in small joints such as fingers and wrists
- Skin rash that especially appears as a red butterfly shape over the nose and cheeks
- You may be sensitive to sunlight which can cause a rash and worsen symptoms
- Mouth ulcers and sores in the nose
- Hair loss
- Kidney problems which can be noticed as foamy urine or swelling in the legs and face
- Psychological symptoms that can manifest themselves in, for example, depression, difficulty concentrating or "brain fog"
- Blood clots which some people with SLE have an increased risk of, especially if they also have antiphospholipid syndrome
What causes SLE?
In SLE, the immune system becomes overactive and misdirected. The exact reason why this happens is not known, but several factors seem to play a role:
- Heredity – the risk of getting SLE increases if someone in the family has the disease
- The body hormone estrogen – about 9 out of 10 people who get SLE are women, often of childbearing age
- Environmental factors – e.g. strong sun, viral infections or smoking
- Certain medicines – can in rare cases trigger SLE-like symptoms, for example certain antibiotics and antiepileptics
How is the diagnosis made?
It can be a challenge to diagnose SLE because the symptoms vary so much. That's why the doctor looks at both how you feel and the results of various tests:
- Blood tests – to see if you have certain antibodies such as S-ANA (Antinuclear antibodies), signs of inflammation or effects on blood cells
- Urine test – to check the kidneys
- Imaging tests – e.g. X-ray or ultrasound for joint or lung problems
- Biopsy – sometimes a tissue sample is taken, especially from the kidneys
How is SLE treated?
There are good treatments that can relieve symptoms, prevent relapses and protect the organs. But there is nothing that can cure SLE.
Common treatments:- Hydroxychloroquine – a basic drug that suppresses the disease and protects against relapses
- Cortisone – used for relapses or if the disease affects internal organs
- Pain-relieving/anti-inflammatory drugs – e.g. for joint pain
- Immunosuppressive drugs – if the disease is more serious, e.g. azathioprine or mycophenolate
- Biological drugs – such as belimumab, for severe or difficult-to-treat SLE
Other important parts in preventing and reducing symptoms are using sun protection because UV light can trigger disease activity. Exercise and good sleep can help with both fatigue and pain. Many people feel good from talking to someone about their disease, so psychological support can also be a good help in managing the disease. In addition, it is important to follow up regularly to be able to detect early if any organ is affected.
Living with SLE can be challenging – but it is possibleWith the right treatment, support and knowledge, most people can live an active and good life. The earlier the disease is detected, the better it can be controlled.
If you suspect that you may have SLE, contact your doctor for further investigation. The sooner you get help, the less risk there is of the disease affecting your organs.