Quick version
The temporomandibular joint is crucial for jaw mobility and is often affected by tension, inflammation or incorrect bites.
- Connects the lower jaw to the temporal bone of the skull
- Enables opening, closing and lateral movements
- Common complaints include pain, clicking sounds and locking
- Affects stress, bite abnormalities and teeth grinding
- Diagnosed with clinical examination and sometimes imaging
What is the temporomandibular joint?
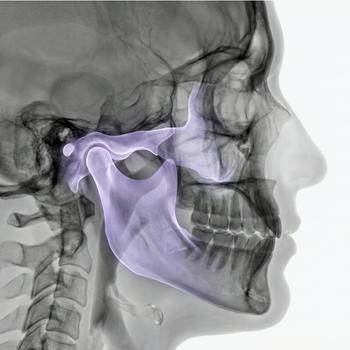
The temporomandibular joint is a double ball-and-socket joint located on both sides of the head where the lower jaw (mandible) meets the temporal bone (os temporale). It has a complex structure with a articular disc (disk) between the joint surfaces that helps control movement and cushion pressure. The temporomandibular joint is unique in that it moves synchronously on both sides during movement and has both hinge and sliding movements.
Anatomy and structure
The temporomandibular joint consists of the mandibular condyle (condylus mandibulae), the mandibular fossa (fossa mandibularis), and a articular disc (discus articularis) between these. Around the joint are ligaments, muscles and a joint capsule that enable and control movement.
Function and movement
The temporomandibular joint allows for several movements, ranging from opening and closing the mouth, lateral movements (laterotrusion) to forward and backward displacement (protrusion and retrusion). These movements are used when you chew, talk, yawn and swallow.
Common causes of temporomandibular joint problems
Problems in the temporomandibular joint can be caused by muscle tension, bite abnormalities, teeth grinding (bruxism), joint inflammation, osteoarthritis or trauma to the jaw. Psychological stress and incorrect movement patterns are also common contributing factors.
Common conditions and diseases
Pain in the temporomandibular joint is often caused by temporomandibular joint dysfunction (TMD), temporomandibular joint osteoarthritis, joint dislocation (dislocation), inflammation or disc displacement. The conditions can lead to pain, noises (clicks), locking or limited opening ability.
Examination and diagnosis
Diagnosis is based on symptoms, clinical examination of range of motion, pain reaction and temporomandibular joint sounds. Imaging diagnostics such as panoramic X-ray, MRI of the temporomandibular joint or CBCT can be used if structural changes or disc problems are suspected.
Relevant symptoms
- Pain when chewing or yawning
- Clicking or cracking noises in the temporomandibular joint
- Locking or difficulty opening/closing the mouth
- Tenderness in the jaw muscles
- Headache or pain around the temple
Related conditions and diagnoses
- Temporomandibular joint dysfunction (TMD)
- Temporomandibular joint osteoarthritis
- Disc displacement in the temporomandibular joint
- Bruxism (teeth grinding)
- Joint dislocation in temporomandibular joint