Quick version
Progesterone is the hormone that literally "settles" the body for a possible pregnancy. Without sufficient levels, it is very difficult for a fertilized egg to attach and develop normally. Therefore, it is not only important to have a functioning ovulation - it is at least as important to see what happens afterwards.
By understanding and gaining insight into your progesterone levels, you will be able to optimize and influence progesterone in order to improve the possibility of a pregnancy. With the right timing, testing and support, you can create the best possible conditions for a successful pregnancy.
Progesterone is not just a "pregnancy hormone" - it is the very key that opens the door to successful fertilization and implantation. Even if ovulation occurs regularly, a lack of progesterone or a too short luteal phase can make it difficult to get pregnant. Understanding your hormonal landscape and in particular the role of progesterone is crucial for many women trying to conceive. With the right knowledge, testing, and possible support, you can optimize your chances for a pregnancy to both occur and develop normally.
What is progesterone and why is it so important for pregnancy?
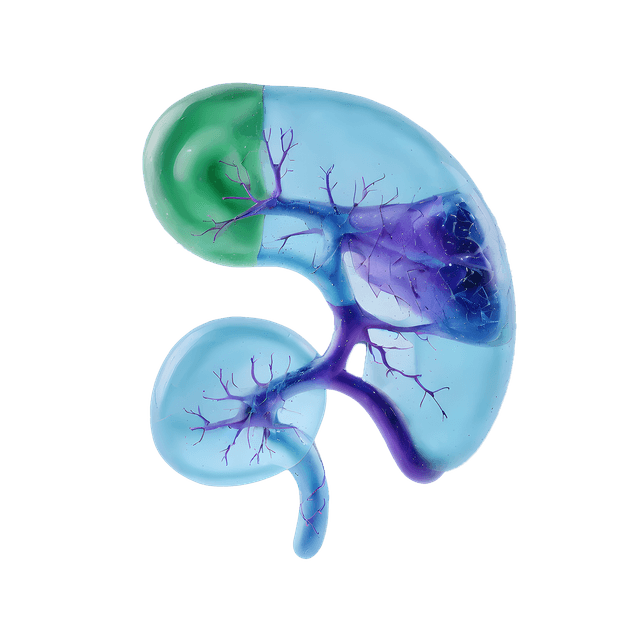
Progesterone is a steroid hormone primarily produced by the corpus luteum in the ovary after ovulation. Because of this, it is often referred to as the corpus luteum hormone. If an egg is fertilized and successfully implants in the endometrial lining of the uterus, the placenta takes over progesterone production around pregnancy weeks 9–10.
Progesterone also plays a critical role in preparing the body even before pregnancy occurs. Already during the luteal phase, directly after ovulation, progesterone creates an environment in the uterus that makes it possible for a fertilized egg to implant. Without sufficiently high progesterone levels during this crucial window, the endometrial lining will not become thick, stable, or receptive enough – which can, in practice, prevent pregnancy from occurring at all.
In other words, progesterone directly influences the ability to become pregnant, not just the ability to maintain a pregnancy. It acts as the body’s signal to the uterus to “prepare the nest” after ovulation. If progesterone levels are too low or the luteal phase is too short, the endometrium may not develop adequately before it begins to shed – which can lead to failed implantation or implantation in an unreceptive environment. Understanding and measuring progesterone during this phase is therefore a crucial part of fertility assessment – especially for women with unexplained infertility, recurrent early miscarriages, PCOS, or irregular cycles.
The role of progesterone before and during early pregnancy
- Prepares the endometrial lining by making it thick, nutrient-rich, and well-perfused – creating the optimal conditions for a fertilized egg to implant and begin to grow.
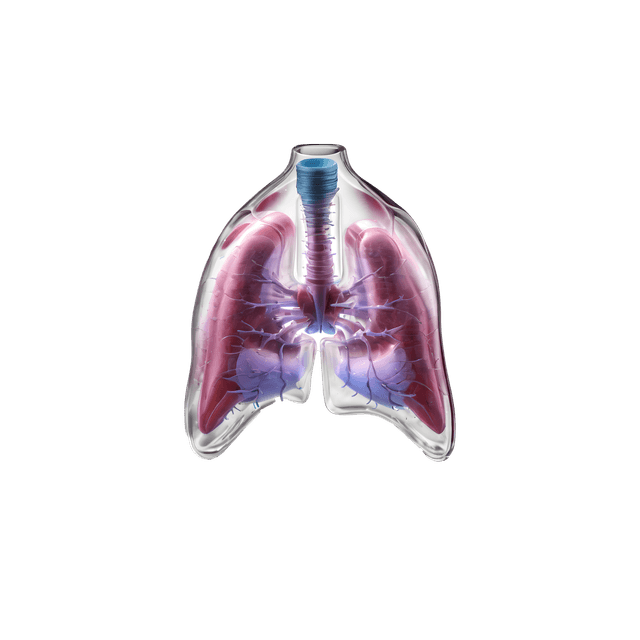
- Helps modulate the maternal immune system so that the embryo, which contains foreign genetic material from the father, is not rejected. Progesterone suppresses specific immune responses, enabling tolerance of the developing embryo.
- Supports uterine muscle stability by reducing contractility. This lowers the risk of the uterus expelling the embryo, thus reducing the chance of early miscarriage.
- Promotes early placental development and function, particularly before the placenta takes over hormone production from the corpus luteum. Adequate progesterone ensures that the placenta can embed into the uterine wall and begin supplying the embryo with nutrients and oxygen.
Progesterone during the menstrual cycle
During the follicular phase (days 1–14), progesterone levels remain low, typically below 3 nmol/L. After ovulation, in the luteal phase (days 15–28), progesterone levels rise rapidly. It is during this phase that the uterus prepares to receive a potential embryo.
Reference values for progesterone when planning pregnancy:
- Follicular phase: < 3 nmol/L
- Luteal phase: ≥ 30 nmol/L is considered favorable for implantation
- Early pregnancy: typically > 60–100 nmol/L
Note: Some laboratories report in ng/mL (1 ng/mL ≈ 3.18 nmol/L).
Low luteal phase levels (< 16 nmol/L) may indicate luteal phase defect, which can reduce the chances of becoming pregnant.
Should you measure your progesterone levels – and if so, when?
Yes, measuring progesterone is an important tool in fertility evaluation – especially if you are struggling to conceive despite signs of ovulation, or if your luteal phase is short (less than 10 days).
When is the best time to test your progesterone levels?
If you want to assess your fertility and test your levels of progesterone, it is essential to take the blood sample at the correct time in your cycle for the result to be accurate.
Follow these guidelines to determine the right time for testing:
- Blood samples are typically recommended about 7 days after ovulation, which in a 28-day cycle usually corresponds to cycle day 21.
- Do you have irregular cycles? Then it is best to first identify ovulation using ovulation tests or by tracking your basal body temperature – and then take the test seven days later.
This is the phase – mid-luteal – when progesterone levels should peak, making it the best time to evaluate whether levels are adequate to support a potential pregnancy.
How to naturally support your progesterone levels
Lifestyle changes- Stress management: Elevated cortisol levels (the stress hormone) can suppress progesterone production.
- Diet: Ensure sufficient intake of zinc, vitamin B6, and cholesterol – all essential for hormone synthesis.
- Healthy body composition: Extreme underweight or overweight can disrupt hormonal balance and ovulation.
- Vitamin B6 and C: May support increased progesterone production.
- Vitex agnus-castus (chasteberry): A plant-based supplement that may help regulate the luteal phase and enhance its function.
- Micronized progesterone: Administered vaginally or orally, often prescribed for confirmed luteal phase defect or during IVF treatment.
- Ovulation-stimulating medications: For example, Letrozole or Clomiphene can help boost ovulation and support corpus luteum function.