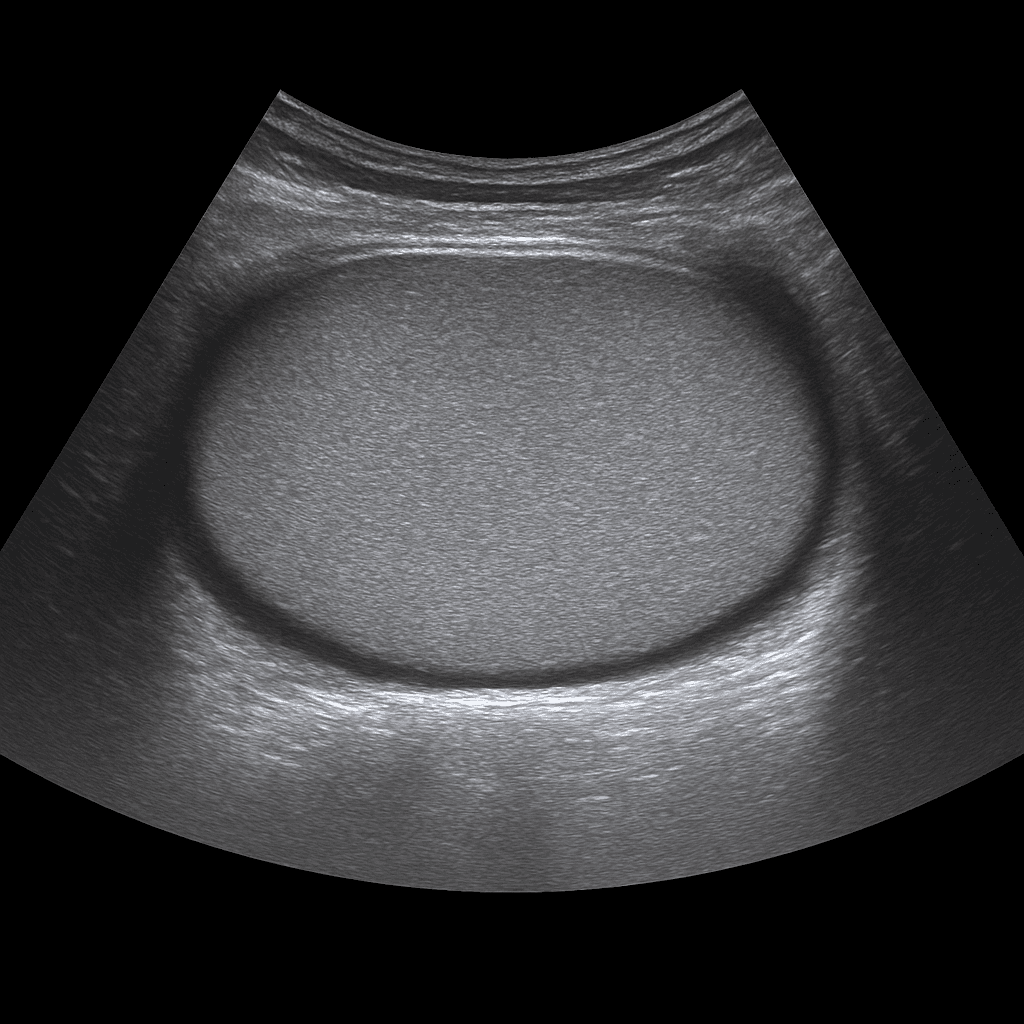
A testicular ultrasound is used to examine the testicles, epididymis and surrounding tissues in the scrotum. The examination is performed by a specialist in radiology and provides detailed images in real time that can show inflammation, fluid accumulation, cysts, blood circulation and possible tumor changes. Testicular ultrasound is the most common method for pain, swelling or a lump in the scrotum.
Testicular ultrasound – for pain, swelling or a lump
The examination is recommended for acute or prolonged pain in the scrotum, sudden swelling, suspected inflammation or when a lump is discovered during self-examination. It is also used for suspected fluid accumulation (hydrocele), varicose veins (varicocele) or inguinal hernia affecting the scrotum.
Common symptoms and questions
- Pain or swelling in the testicle or scrotum.
- Lump in the testicle – suspected cyst or tumor.
- Suspected epididymitis.
- Fluid accumulation (hydrocele) or varicose veins (varicocele).
- Suspected testicular torsion – especially in case of acute pain.
- Inguinal hernia affecting the scrotum.
Conditions that can be detected with ultrasound of the testicles
- Epididymitis or testicular inflammation (orchitis).
- Hydrocele – fluid around the testicle.
- Varicocele – varicose veins in the scrotum.
- Torsion – twisting of the testicle that requires urgent assessment.
- Cysts or benign changes.
- Tumor or suspected malignant change in the testicle.
How an ultrasound of the testicles is performed
The examination is performed while you lie on your back. A gel is applied to the skin and the doctor moves the ultrasound probe over the scrotum to assess the testicles and epididymis in detail. The examination takes about 10–15 minutes, is completely painless and requires no special preparation. If necessary, blood flow can be studied using Doppler technology to detect torsion or circulatory disorders.
Order an ultrasound examination of the testicles - get a report and recommendation from a doctor
The images are reviewed by a specialist in radiology who draws up a written medical report. The answer is delivered digitally within a few working days and can be shared with your treating doctor or urologist for further follow-up. If necessary, the examination can be supplemented with MRI for more detailed mapping.