Quick version
Inflammation of the pancreas, known as pancreatitis, is a serious condition that often causes pain in the upper abdomen, nausea, and fever. The most common causes are gallstones and alcohol, but several other factors can be involved. Early diagnosis with blood tests and imaging is crucial for proper treatment and to reduce the risk of complications and recurrence.
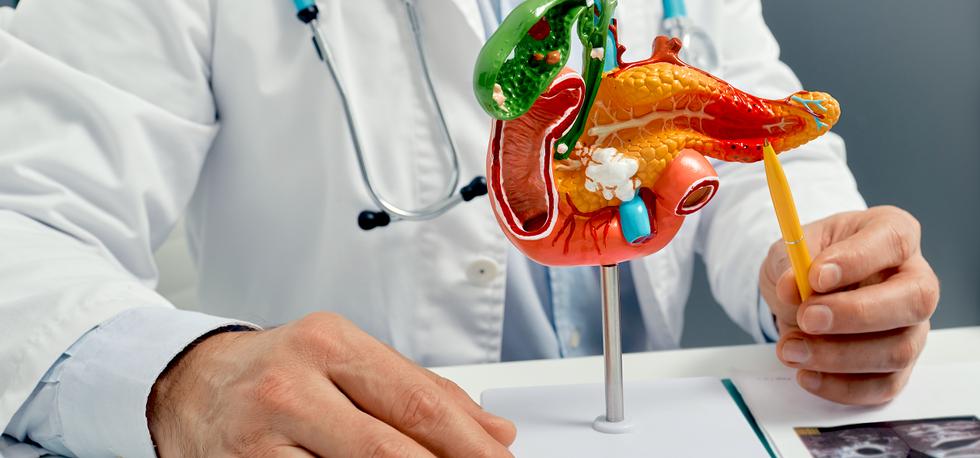
The pancreas produces digestive enzymes that are normally first activated in the intestine. In pancreatitis, these enzymes are activated too early, already in the pancreas, which leads to the glandular tissue starting to break down and become inflamed. This can cause severe pain and affect both digestion and metabolism.
Acute pancreatitis
Acute pancreatitis usually begins suddenly and produces clear, often severe symptoms. The condition is characterized by an acute inflammation in which the pancreatic digestive enzymes are activated prematurely and cause tissue damage. The pain is generally localized to the upper abdomen and may radiate to the back, often in combination with nausea, vomiting and fever.
In many cases, the inflammation is mild and self-healing with the right supportive treatment, but acute pancreatitis can also become serious. In more severe forms, the inflammation can lead to severe fluid loss, circulatory problems and effects on other organs such as the kidneys and lungs. There is also a risk of local complications such as necrosis, fluid accumulation and infections in or around the pancreas.
Acute pancreatitis always requires medical assessment and often hospitalisation for monitoring, pain relief and fluid therapy. Early identification of the underlying cause, such as gallstones or alcohol, is important to reduce the risk of recurrence and to prevent future complications.
Chronic pancreatitis
Chronic pancreatitis develops gradually and involves long-term, often recurring inflammation that gradually leads to permanent damage to the tissue of the pancreas. The inflammation causes normal glandular tissue to be replaced by scar tissue (fibrosis), which impairs the pancreas' ability to produce digestive enzymes and hormones.
Over time, this can lead to exocrine pancreatic insufficiency, where the breakdown of fat, protein and carbohydrates becomes insufficient. The result can be diarrhea, fatty and foul-smelling stools, bloating, malabsorption and involuntary weight loss. At the same time, the hormone-producing part of the pancreas can be affected, which increases the risk of developing diabetes.
The pain of chronic pancreatitis varies. Some have long-term, dull abdominal pain, while others experience intermittent episodes of pain or gradually decreasing pain as nerve structures are damaged. Chronic pancreatitis is a condition that requires long-term follow-up and treatment with pain relief, enzyme replacement, nutritional support and treatment of underlying causes.
Common symptoms of pancreatitis
The symptoms of inflammation of the pancreas vary depending on whether the condition is acute or chronic, but common symptoms are:
- Pain in the upper part of the stomach, often radiating to the back.
- Nausea and vomiting.
- Fever.
- Loss of appetite.
- Bloating and tenderness in the abdomen.
In chronic pancreatitis, symptoms may be more diffuse and manifest as long-term abdominal pain, fatty and foul-smelling stools, and involuntary weight loss.
Common causes of pancreatitis
The two most common causes of pancreatitis are gallstones and alcohol, but several other factors can contribute.
Gallstones
Gallstones can block the bile and pancreatic ducts, which prevents digestive enzymes from emptying normally and instead causes inflammation of the pancreas.
Alcohol
Long-term or heavy alcohol consumption is a common cause of both acute and chronic pancreatitis. Alcohol can directly damage pancreatic cells and disrupt enzyme balance.
Other causes
Inflammation of the pancreas can also be caused by medications, high triglycerides, severely elevated calcium, infections, autoimmune conditions or in some cases be idiopathic, that is, without a clearly identifiable cause.
How is pancreatitis diagnosed?
Diagnosis is based on a combination of symptoms, laboratory tests and imaging. If pancreatitis is suspected, blood tests are often the first step.
Blood tests
Elevated levels of pancreatic amylase and lipase are typical in acute pancreatitis. Inflammatory markers and electrolytes are also analyzed to assess the severity of the disease.
Imaging
Ultrasound, computed tomography (CT) or Magnetic Resonance Imaging Pancreas can be used to identify the cause of the inflammation, such as gallstones, and to assess complications.
Treatment and follow-up
The treatment of pancreatitis depends on the cause and severity. Acute pancreatitis often requires hospitalization with pain relief, fluid therapy, and fasting to relieve the pancreas. In cases of pancreatitis caused by gallstones, surgery may be necessary. In cases of chronic pancreatitis, treatment focuses on pain relief, enzyme supplements, nutritional support, and treatment of the underlying cause.
How can the risk of new inflammation be reduced?
The risk of recurrent pancreatitis can be reduced by treating underlying causes. This may mean helping the gallbladder in case of gallstone disease, abstaining from alcohol, treating elevated blood lipids and following medical advice in case of drug-induced pancreatitis.