Quick version
High blood lipids are common and increase the risk of cardiovascular disease over time. Reference ranges are used as a guide, but many specialists now advocate lower LDL levels, often below 3.5 mmol/L, to reduce long-term risk. Blood lipids are influenced by both genetic factors and lifestyle, which means that the starting point and response vary between individuals. Lifestyle changes in physical activity, diet, weight, sleep and stress can improve lipid status and the overall risk profile, but always need to be assessed individually.
Reference ranges for cholesterol are intended as a guide, not as absolute risk limits, and should always be interpreted individually. Many cardiologists today advocate lower LDL levels than before, often below 3.5 mmol/L, to reduce the long-term risk of cardiovascular disease – although there is not full agreement on exact target values and, not least, when treatment is necessary. For those with elevated cholesterol levels or test results in the grey zone, the question therefore arises as to which measures can actually affect the risk picture over time.
What is meant by high blood lipids?
Blood lipids, also called lipids, consist of several different components, but the main ones used are total cholesterol, LDL cholesterol, HDL cholesterol and triglycerides. These values reflect different aspects of the body's fat metabolism and have varying significance for the risk of developing cardiovascular disease.
Of these, LDL cholesterol has long had a central role in risk assessment, since elevated levels are linked to the deposition of cholesterol in the walls of blood vessels and the development of atherosclerosis over time, whereupon it is also popularly referred to as the "bad" or "evil" cholesterol.
At the same time, lipid status is more than a single number. The distribution between different blood fats, the presence of other risk factors and the individual risk profile are always at least as important as a single value.
Why are elevated blood fats so common?
The fact that elevated blood fats are common is rarely due to a single factor. In most cases, it is the result of an interaction between genetic vulnerability and lifestyle-related factors. Heredity plays a significant role – some people have a genetic predisposition to produce more LDL cholesterol or to break down and clear cholesterol from the bloodstream more slowly.
In these individuals, lipid levels can be elevated already at a younger age, sometimes despite an otherwise healthy lifestyle. This means that two people with similar lifestyles can have completely different lipid profiles, depending on genetic predispositions.
At the same time, blood lipids are greatly influenced by lifestyle. Dietary patterns, physical activity, body weight and metabolic health are of great importance. Factors such as insulin resistance, abdominal obesity and low physical activity levels are often linked to elevated triglycerides, lower HDL and a more unfavorable LDL profile.
Other lifestyle factors also contribute. Long-term stress, lack of sleep and smoking can negatively affect fat metabolism, as can regular high alcohol intake. In a society where sedentary lifestyle is common and energy-dense, processed food is readily available, it is therefore not surprising that elevated blood lipids have become a public health problem.
It is precisely this combination of biological conditions and modern lifestyle habits that makes high blood lipids so common – and which also explains why measures need to be individually adapted.
Is it possible to influence blood lipids with lifestyle changes?
In many cases, it is possible to influence lipid status through lifestyle changes. However, the extent of the effect varies significantly between individuals and depends on factors such as genetic background, starting levels, metabolic health and how consistent the changes are over time.
Some people can see clear improvements in LDL, triglycerides and HDL after relatively small adjustments, while others – despite extensive efforts – achieve more limited changes in their values. This reflects the large individual variation in how the body regulates blood lipids.
Lifestyle changes can affect blood lipids through several different mechanisms, including:
- regular physical activity.
- changed dietary patterns.
- weight loss in case of overweight or abdominal obesity.
- improved insulin sensitivity.
- reduced stress and better sleep.
- smoking cessation and moderate alcohol consumption.
Lifestyle changes should therefore be seen primarily as a way to improve the overall cardiovascular risk profile over time, rather than as a guarantee of reaching an individual target value. Even modest improvements can have clinical significance when several risk factors are affected simultaneously.
Physical activity and blood lipids
Regular physical activity is one of the most effective lifestyle factors for improving the lipid profile. Exercise is particularly linked to lower triglycerides and higher HDL cholesterol, while the effect on LDL is often more moderate.
Both cardio and strength training have positive effects. The key is continuity – even moderate, regular exercise can produce measurable improvements over time.
The role of diet in lipid balance
The impact of diet on blood lipids is individual and complex. For some, reducing saturated fat intake leads to clearly lower LDL levels, while others respond less to the same changes.
Dietary patterns that are often associated with improved lipid status include:
- higher intake of fiber-rich foods.
- less ultra-processed foods.
- switching from saturated to unsaturated fats.
- lower intake of sugar and refined carbohydrates, especially if you have high triglycerides.
There is no universal cholesterol-lowering diet that suits everyone. Dietary advice should therefore always be adapted to the individual's starting point and metabolic conditions.
Weight, insulin resistance and triglycerides
Overweight, especially abdominal obesity, and insulin resistance are strongly linked to an unfavorable lipid profile. In these contexts, high triglycerides and low HDL are often seen, even when LDL is only moderately elevated.
Even a limited weight loss can produce clear improvements in blood lipids, especially through reduced insulin resistance.
Other lifestyle factors to consider
In addition to diet and exercise, lipid status is also affected by other factors:
- smoking, which lowers HDL and increases vascular risk.
- prolonged stress and insufficient sleep.
- alcohol consumption, which can raise triglycerides.
Taking these factors into account is important for the overall cardiovascular risk, although the effect on individual lipid values varies.
When are lifestyle changes not enough?
For some people, especially with pronounced heredity or very high LDL levels, lifestyle changes are not enough to reach recommended levels. In these cases, drug treatment may be necessary to reduce the long-term risk of cardiovascular disease.
However, lifestyle changes always constitute an important basis – even with medical treatment – because they affect several risk factors simultaneously.
High cholesterol – common but often undertreated
High cholesterol is common in Sweden but both underdiagnosed and undertreated. Studies show that a significant proportion of adults, especially men, have elevated cholesterol levels in combination with high cardiovascular risk – even though many already qualify for treatment. The figure illustrates the proportion of people with high cholesterol, and how this differs between women and men.
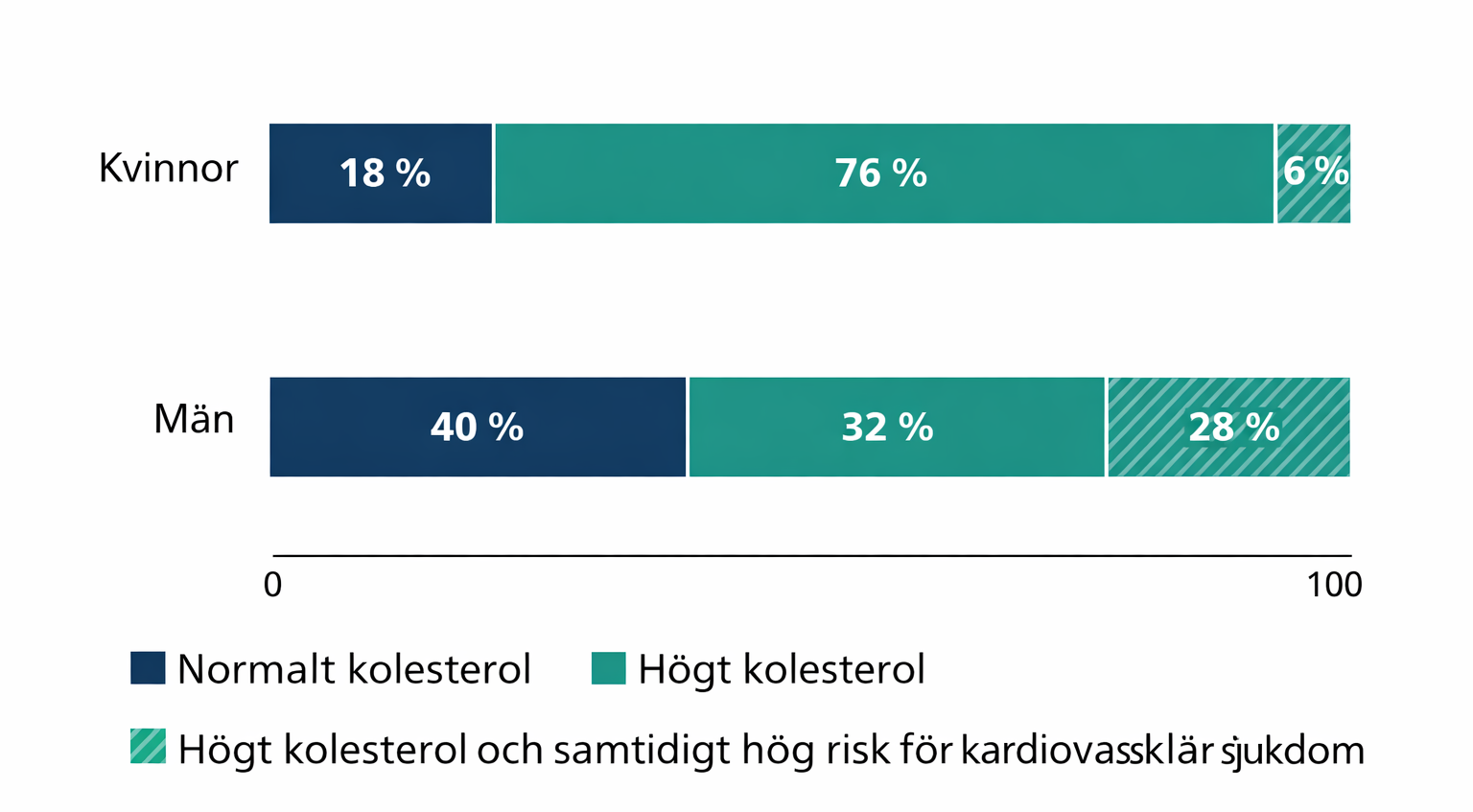
The information in the diagram is based on data from the Stockholm Diabetes Prevention Program (SDPP) and the National Board of Health and Welfare's drug register. The studies show that a significant proportion of adults in Stockholm County have high cholesterol, and that men in particular more often combine elevated cholesterol levels with high cardiovascular risk according to SCORE.